Mental Health Teams Ignore Family Concerns and Fail to Detain Masking Patients
Some (not all) sufferers of severe mental illnesses like schizophrenia and bipolar learn to mask their symptoms when faced by medical…

Raise awareness, fill the compassionate gap and sign the petition.
Some (not all) survivors of severe mental illnesses like schizophrenia and bipolar disorder learn to mask their symptoms when assessed by healthcare professionals.
This is not just a coping skill consequence of paranoia or distrust, it is a survival defence to avoid the involuntary but necessary interventions formed to help them. This masking exacerbates the survivor's symptoms as help goes unused and the condition heightens.
I’ve seen this happen with two close family relatives of mine, one of them being my mother.
Please note this is an incredibly sensitive topic for me to write about. I am only deciding to publish this article because I’m depleted and at my wits’ end.
This essay is NOT for idle gossip or to expose the survivors to ridicule. It serves as a record of evidence and the impact of systemic neglect. If you read with this essay, please honour the intended purpose. Highlight the vital need for mental healthcare reform in the UK, not on the survivors whose pain was laid bare.

We, the family, witness these sufferers in the midst of a suspected psychotic episode. They’ll accuse strangers on the street of muttering disparaging things at them; they’ll open windows and shout weird onomatopoeic sounds to the public; they’ll drag people out of cars or smash windows. A blatant display of their deteriorating mental health which is abundantly obvious to those who interact with them daily, their friends and family.
However, they, the healthcare professionals, come across a different person. They visit the sufferers for a limited time slot, “assess” their condition, and because the sufferers mask and answer the questions in a coherent, engaged and lucid manner, the fundamental reality of their condition is entirely missed.
When questioned about their mental state by the professionals, the sufferers in false sincerity answer, “No, I don’t intend to harm myself,” or “No, I don’t hear or see things that aren’t there.”
All of a sudden, the family concerns, the emails sent and reports made are thrown out and dismissed in favour of a brief, masked denial.
“My mother has literally told me she wants to 'end her life' multiple times.
What are you talking about she has said 'no, she doesn’t.' Why are you believing that? If you were paranoid and had distrust in everyone, would you readily admit to medical strangers sent to assess you, ‘Oh yes, I do intend to harm myself. and I do hear things that aren’t there.’ No, you wouldn’t. Please use discernment and common sense.” I passionately state down the phone to a mental health professional.
“She wouldn’t have been able to mask her condition for an hour.” The professional retorts.
“Yes, you could. If you’ve been undiagnosed for so long and coping with such a condition with no help for two decades,” I say.
“Also, there is family history of diagnosed severe mental conditions. Do you not take that into consideration?”
The professional falls silent at these common-sense statements.
Since I was a child, my mother would accuse people on the street of calling her a “hoe.” She would argue with every parent at the primary school gate and get into arguments or fights.
Her paranoia and suspected auditory hallucinations were so turbulent that she changed my nursery and primary schooling every year because of this (except for the last one, where I somehow stayed for two or three years.)
In anguish, at home, she would talk to herself incessantly, go on about conspiracies I did not understand (and still don’t), and accuse people of being “Badmind.” She would open the windows and doors and make weird noises to passersbys. Her moods would switch from rage to despair every few minutes.

Now, I, as an adult — a mother at 24 years old, with my own daughter — my siblings and I have tried desperately to get my mother the mental help she desperately needs.
(The help she’s needed for at least 20 years in mine and my brother’s view).
Yet, the NHS mental health systems fail continuously. They instead rank a brief assessment interview under the Mental Health Act by healthcare professionals who only know her for an hour, over decades of lived experience and ever growing concerns from her family members (and even some outside professionals.)
The other family member I aforementioned has a diagnosis of schizophrenia and gets sectioned every year. To note, said family member only gets sectioned after committing crimes or disturbing the public to a point that requires police to intervene, rather than the medical professionals fulfilling their Duty of Care part during assessments.
The professionals will see said family member on Monday after reports from family or friends, they will conduct their assessment, and because the said family member engaged, “I feel fine,” they will dismiss any further concerns. The next day, said family member is being arrested for disturbing the public and is sectioned there and then.
This illustrates that the only way for the current mental health system to validate the illness is through public disturbance or criminal act, not clinical assessment.
Said family member has been sectioned every single year for ten years straight, usually through arrests as MHA assessments fail.
Last year, the mental health team themselves confessed they were failing this family member and, as a result, they prolonged their in-patient sectioning in 2024, stating they needed to “evaluate how they have been failing them for so long evident by yearly repeated sections and their condition seemingly not being managed or improving.” That’s their own admission of inadequacy.
Nonetheless, this type of systemic failure to safeguard is at the hands of police, too. Though yes, they have been able to section said diagnosed family member year in and year out, I remember one hot night in July 2022 when police were called in absolute dire urgency as this family member was being particularly threatening and hostile to others.
The police dispatch said they would send officers out. Two or three hours later, we see a police car drive by the house with no sirens on. We frantically call back to ask why no one has turned up. Their response, “no officers available.”
A bold faced lie. It took contacting the crisis team, who then had to contact the police themselves, to finally get this family member the medical and mental health attention they needed. What an inexcusable, to put it bluntly, disgusting, and negligent pattern. A family’s concern is dismissed, which is clearly paramount in these social and mental care services.
Those who are meant to protect do not do so because the system that trains the professionals fails to take into account for high-level masking presentation.
Professionals are urged to make critical decisions in an insufficient hour timeframe. High-level masking is victorious in this timeframe despite the belief to the contrary. I have two family members who are absolute proof of this.
Here’s how it goes: professionals conduct an insufficient Mental Health Act assessment where sufferers mask highly, they believe the masking and dismiss any family concerns, the sufferer either goes on suffering or is detained at a later date because the crisis results in public disturbance where police intervene.
We need reform now. We, the loved ones who are much more intimately aware of these episodes, demand the immediate prioritisation of family lived experiences and evidence.
The fear that my mother will become another case study of systemic neglect, despite mounting concerns from her family, is unbearable. Depleting. Heart-wrenching.
As I begin my Master's in Psychology (Conversion) next year 🧿, this type of systemic negligence and miseducation, (along with my own diagnosed neurodivergence OCD and ARFID), is the motivation and purifying fire behind my career prospects.
Things must change! We need a system that recognises that the most severe form of suffering is often masked by some survivors. We need a system that prioritises and takes multiple family members' concerns on board. We need a system that is well-informed by experience rather than just relying on textbook analysis.
I am working on writing a UK Government Petition for this exact matter. I will include the link in this article once it’s up.
Update on the UK Government Petition: I wrote a petition on 15th November 2025 but in January 2026, it was rejected as they accepted another petition with the same aims a few days prior (so myself and the other petitioner likely wrote it at the same time as petitions run for 6 months, and their one finishes July 2026).
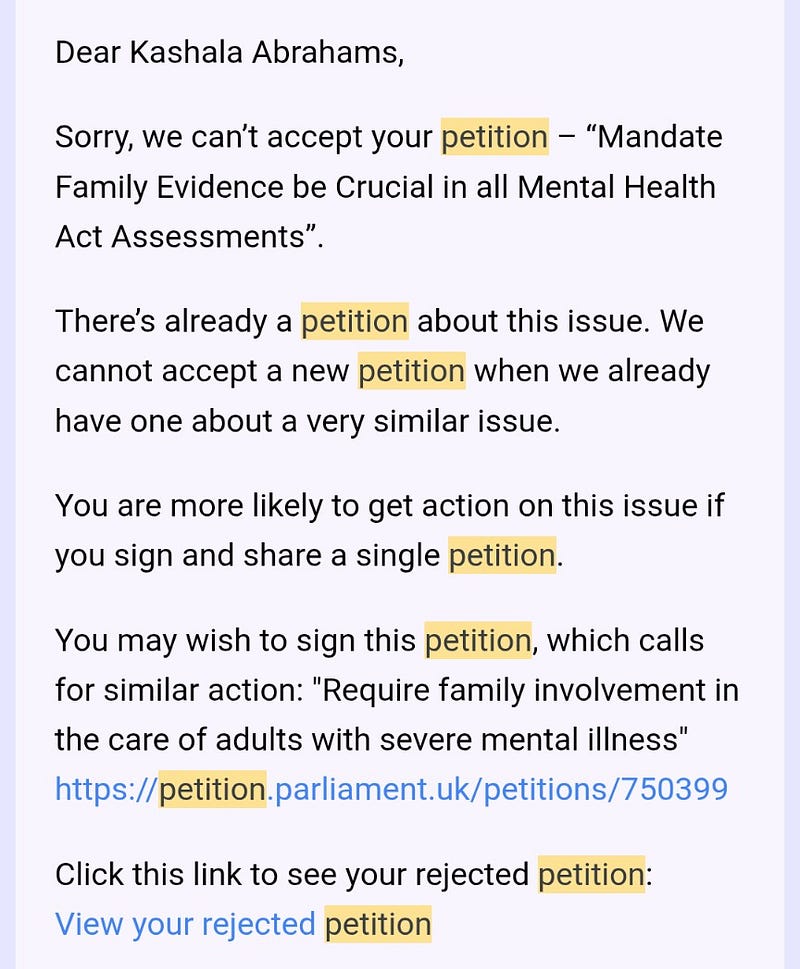
Here’s a link to that petition by Davis: https://petition.parliament.uk/petitions/750399